A Chemoport is a small medical appliance that is installed beneath the skin. A catheter connects the port to a vein. Under the skin, the port has a septum through which drugs can be injected and blood samples can be drawn many times, usually with less discomfort for the patient than a more typical “needle stick”. Ports are used mostly to treat hematology and oncology patients. The port is usually inserted in the upper chest, just below the clavicle or collar bone, leaving the patient’s hands free.
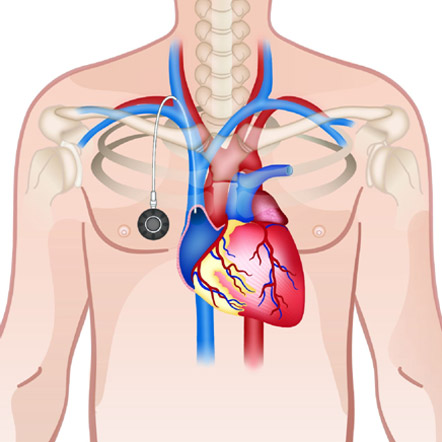
A port consists of a reservoir compartment (the portal) that has a silicone bubble for needle insertion (the septum), with an attached plastic tube (the catheter). The device is surgically inserted under the skin in the upper chest or in the arm and appears as a bump under the skin. It requires no special maintenance and is completely internal so swimming and bathing are not a problem. The catheter runs from the portal and is surgically inserted into a vein (usually the jugular vein or subclavian veins). Ideally, the catheter terminates in the superior vena cava, just upstream of the right atrium. This position allows infused agents to be spread throughout the body quickly and efficiently.
No. The mediport placement procedure is a minimally invasive procedure. You will only receive local anesthesia with some sedation and pain control medication if you need it during the procedure.
You will have two small incisions that were necessary for placing the port. The smaller one is in the neck and is about 5 mm. The other incision is in your chest wall and is about 2 cm. Both incisions were closed with stitches and/or glue.
You should expect some bruising, swelling, and tenderness to the area of your body where the port is placed. These symptoms usually go away gradually over the next 5 to 7 days. You may take pain killers and antibiotics if you are not allergic to these medicines for relief of the discomfort and prevent infections.
- Infection.
- Thrombosis: Formation of a blood clot in the catheter may block the device irrevocably. To prevent clotting the Chemoport is flushed with saline and heparin, usually by a nurse or other medical professional, or a properly trained family member or the patient, at least once every four weeks, or more often in conjunction with administering medication.
- Age: If the device is put into a child, the child’s growth means that the catheter becomes relatively shorter and will move away from the inferior part of the superior vena cava. It might be necessary to remove or replace it.
- Pneumothorax: Attempts to gain access to the subclavian vein or jugular vein can injure the lung, possibly leading to this complication. If the pneumothorax is large enough, a chest tube might need to be placed. In experienced hands, the incidence of this complication is about 1%.
- Arterial injury: The subclavian artery can be inadvertently punctured. This usually leads to a subcutaneous hematoma and occasionally a pseudoaneurysm. An alternative site may need to be used for port placement. Puncture of the carotid artery is rarer, since attempts to access the nearby jugular vein are done in our institution with ultrasound guidance.
- Leave the dressing in place for 24 hours. After 24 hours, if you have stitches, then do the following:
- Remove the dressing over the stitches and clean around the incision with a well wringed out soapy clean washcloth.
- Avoid washing the incision itself.
- Pat the area dry.
- Do not scrub.
- Apply fresh, sterile 4 inch x 4 inch gauze dressing over the site after cleaning and replace every day for 7 days.
- Keep the site dry and avoid getting this area wet during showers. Delay baths until physician approval, which will be about 10-14 days.
Your port will be flushed with a fluid after each use to keep the Chemoport working. If your port is not being used, it should be flushed every 4 weeks to maintain it. This is most often done by a health care professional. If you or your family needs to do this, a nurse will teach you.
You must keep all stitched sites and dressings dry while bathing and showering. Here is how:
- Carefully cover the incision and dressing with plastic wrap like Saran wrap.
- Apply the wrap to cover the entire incision and dressing.
- Use tape to seal the edges all around so that no water runs behind the plastic wrap.
- After the shower, remove the plastic wrap and dressing. This is the best time to clean and redress the sites.
- No swimming or immersing the port site until approved by your physician.
- Be gentle with the incisions. Do not let the water beat on them.
Increased bruising, swelling, tenderness, more redness or pain at your incision sites, fever or chills, increased bleeding or drainage from your incisions, or any problem or concerns or unusual symptoms with your port should be reported.
Once your port is no longer needed for your treatment and vascular access needs, we can remove your port in our department in a room similar to the one you were in today for the port placement.
The port should not change your daily activities. Avoid strenuous exercises for a few weeks after surgery, so that the body can heal. Avoid hitting the port against anything. Your doctor or nurse will answer any questions you have about resuming your normal activities. When in doubt, seek medical attention. Continue seeing your doctors. Call them to make an appointment if you do not already have an appointment.
