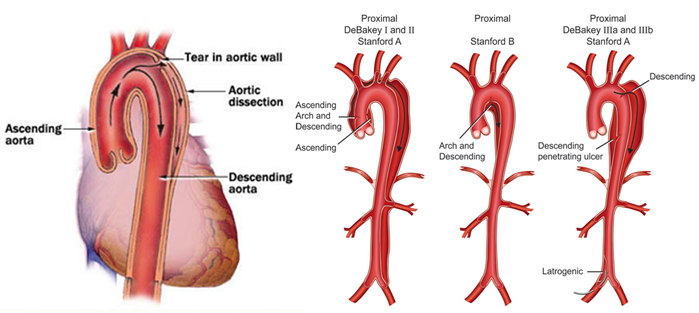
Aortic dissection is the most common catastrophe affecting the aorta. The aorta is the largest artery of the body through which blood leaves the heart to deliver oxygenated blood to the rest of the body. It is caused when the inner layer of the aortic wall tears and then peels or separates away from the next layer of the aorta. This creates two channels; the original aortic channel for blood flow (the true lumen) is still present while the peeling away of the outer layer in the dissection creates a new additional flow channel (the false lumen).
This double-barrel flow pattern in the dissected aorta can cause serious problems upstream or downstream from the tear. The dissection or separation can result in a significant decrease in blood flow to various organs and tissues supplied by the involved branches. Branches that may be affected include the kidney (renal) arteries, the gut (mesenteric) arteries, the arteries to the brain, and the arteries to the arms or legs. In addition, the tear may compromise blood flow to the heart causing a heart attack and in some cases can result in internal bleeding around the heart, causing loss of consciousness or death. Aortic dissection is a very serious, life-threatening disorder that requires immediate medical attention.
Risk Factors
The main preventable risk factor for an aortic dissection is high blood pressure (hypertension). Over time, hypertension weakens the aortic wall, making it more likely to have a spontaneous tear involving the inner lining of the aorta. The tear exposes the middle of the wall to very high aortic blood pressure. This creates a separation that unzips the aorta between the layers which are pulled apart by the dissection process, leading to the double-barrel flow pattern. Other risk factors for aortic dissection include: Marfan or Ehlers-Danlos syndrome, which are inherited disorders of blood vessels and connective tissues; presence of aortic aneurysm or enlargement of the aorta; a family history of aortic dissection; and certain heart conditions such as a bicuspid aortic valve. Aortic dissection may also occur as a complication of open heart surgery or heart catheterization, although this is very rare.
Aortic dissection symptoms may be similar to those of other heart problems, such as a heart attack. Typical signs and symptoms include:
- Sudden severe chest or upper back pain, often described as a tearing, ripping or shearing sensation, that radiates to the neck or down the back
- Loss of consciousness
- Shortness of breath
- Sudden difficulty speaking, loss of vision, weakness or paralysis of one side of your body, similar to those of a stroke
- Weak pulse in one arm compared with the other
When a physician suspects the diagnosis of aortic dissection, an imaging test is generally ordered to evaluate the aorta. There are three primary tests used to diagnose aortic dissection. Aortic dissection can be diagnosed with a CAT scan of the aorta or an MRI scan. A transesophageal echo (TEE) may also be performed. A TEE is a special type of ultrasound test during which a small ultrasound probe is passed through the mouth and into the stomach and esophagus to take very detailed pictures of the heart and aorta. Currently there are no blood tests that can accurately diagnose aortic dissection.
Because of the potentially fatal nature of aortic dissection, patients are treated immediately. Drugs are administered to reduce the blood pressure and heart rate. If the dissection is small, drug therapy alone may be used. In other cases, surgery is performed.
In surgery, damaged sections of the aorta are removed and a synthetic graft is often used to reconstruct the damaged vessel. The objective in the surgical management of aortic dissection is to remove the most severely damaged segments of the aorta, and to eliminate the entry of blood into the tear. While excision of the tear may be performed, it does not significantly change mortality.
Some methods of repair are:
- Replacement of the damaged section with a tube graft when there is no damage to the aortic valve.
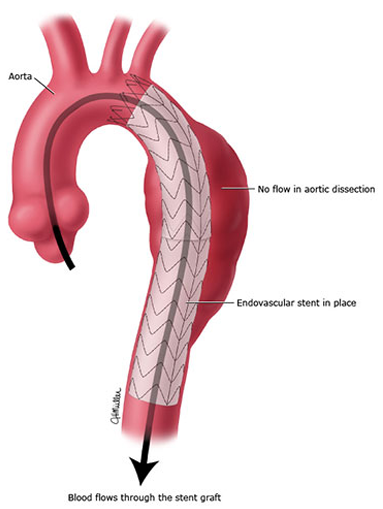
- Insertion of a stent graft (covered stent), e.g. in TEVAR (thoracic endovascular aortic repair). It is usually combined with on-going medical management
- Replacement of the damaged section of aorta with a sutureless vascular ring connector-reinforced graft. Vascular ring connector (VRC) is a titanic ring used as a stent in the vascular graft to achieve a quick, blood-sealed, and sutureless connection.
In an acute dissection, treatment choice depends on its location. For Type A dissection, surgery is preferred over medication. For uncomplicated Type B (distal aortic) dissections, medical management is preferred over surgical.
The risk of death due to aortic dissection is highest in the first few hours after the dissection begins, and decreases afterwards. Because of this, the therapeutic strategies differ for treatment of an acute dissection compared to a chronic dissection. An acute dissection is one in which the individual manifests symptoms of dissection within the first two weeks. If the individual has managed to survive this window period, his prognosis is improved. About 66% of all dissections present in the acute phase. Individuals who present two weeks after the onset of the dissection are said to have chronic aortic dissections. These individuals can be treated with medical therapy as long as they are stable.
Aortic dissection generally appears as a hypertensive emergency, and the prime consideration of medical management is strict blood pressure control. Beta blockers are a first line treatment for patients with acute and chronic aortic dissection. Vasodilators such as sodium nitroprusside can be considered for patients with ongoing hypertension, but they should never be used alone, as they generally cause reflex tachycardia.
For all patients who have an aortic dissection longterm follow-up with a physician is a very important part of treatment. Blood pressure and heart rate need to be carefully monitored and controlled with medications. For many patients, CAT scans or MRI scans will be repeated at regular intervals (such as every 6 months or every year) to monitor the size of the aorta and the status of the dissection.