Hematuria is the presence of red blood cells (erythrocytes) in the urine. It may be idiopathic or benign, or it can be a sign that there is a kidney stone or a tumor in the urinary tract (kidneys, ureters, urinary bladder, prostate, and urethra), ranging from trivial to lethal.

Blood in the urine is a symptom – not a specific condition – and happens when part of your urinary tract, often your kidneys, allows blood to leak into your urine. There are a number of reasons why blood may appear in the urine:
- Urinary tract infection (UTI)
- Kidney infection
- Kidney or bladder stones
- BPH (benign prostatic hyperplasia, or an enlarged prostate)
- Kidney disease
- Cancer
- Certain medications
- Injury to the kidneys
- Inherited disorders
Since the introduction of percutaneous renal biopsy, the procedure has provided important information for the diagnosis, management and prognosis of many patients with renal diseases. However, this procedure is not free from complications. Although >90% of patients after renal biopsy have CT-detectable haematomas, bleeding requiring transfusion or other clinical intervention occurs in only 1–6% of patients. Renal bleeding has been associated with intrarenalarterio-venous fistulas (AVFs), which are known to be a major complication of renal biopsy. AVFs can be demonstrated by arteriography in up to 15% of patients, and the frequency is high in renal allografts. This complication may remain asymptomatic and resolve spontaneously, or lead to renal bleeding, uncontrollable hypertension and/or deterioration of renal function. These are features that may require correction, and selective embolization with coaxial catheterization is known to be the most effective and non-invasive method of AVF treatment with minimal renal parenchymal damage.
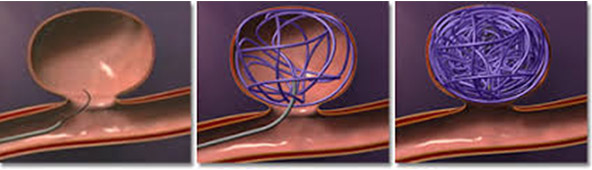
It is a minimally invasive technique performed by an interventional radiologist. The interventional radiologist inserts a catheter into the patient’s femoral vein (in the upper thigh) using fluoroscopy for guidance. The interventional radiologist then directs the catheter to the affected arteriesresponsible for hematuria due to traumatic cause and inserts embolisation materials/coils into the distal braches of arteries responsible for the bleeding to block the area, stopping the bleeding. The patient will have an angiography after the embolisation procedure to confirm if the procedure has been successful. The treatment has high rates of immediate clinical success.

You will already have undergone some tests including a computed tomography (CT) scan to identify the area of bleeding.You will be an inpatient for the procedure. You may be asked not to eat for four hours before the procedure. If you have any allergies or have previously had a reaction to the dye (contrast agent), you must tell the radiology staff before you have the test.
A specially trained team led by an interventional radiologist within the radiology department. Interventional radiologists have special expertise in reading the images and using imaging to guide catheters and wires to aid diagnosis and treatment.
In the angiography suite or theatre; this is usually located within the radiology department. This is similar to an operating theatre into which specialised X-ray equipment has been installed. a
You will be asked to get undressed and put on a hospital gown. A small cannula (thin tube) will be placed into a vein in your arm. The procedure will take place in the X-ray department and you will be asked to lie flat on your back. You may have monitoring devices attached to your chest and finger and may be given oxygen. Your groin area will be swabbed with antiseptic and you will be covered with sterile drapes. Local anaesthetic will be injected into the skin in your groin and a needle will be inserted into the artery. A fine plastic tube called a catheter will be placed into the artery. The radiologist uses X-ray equipment to guide the catheter towards the arteries that are responsible for hematuria due to traumatic cause. A special X-ray dye (contrast agent) is injected into the catheter to ensure a safe position for embolisation. The interventional radiologist can then block the abnormal arteries by carefully inserting metallic coils through the catheter guided by images on a screen. Small amounts of contrast are injected down the catheter to check that the abnormal arteries are blocked satisfactorily. Once the interventional radiologist is satisfied with the images, the catheter will be removed. Firm pressure will be applied to the skin entry point, for about ten minutes, to prevent any bleeding. Sometimes a special device may be used to close the hole in the artery.
Every patient is different, and it is not always easy to predict; however, expect to be in the radiology department for about two hours.
You will be taken back to your ward. Nursing staff will carry out routine observations including pulse and blood pressure and will also check the treatment site. You will stay in bed for at least six hours. You will be kept in hospital overnight and may be discharged the next day.
