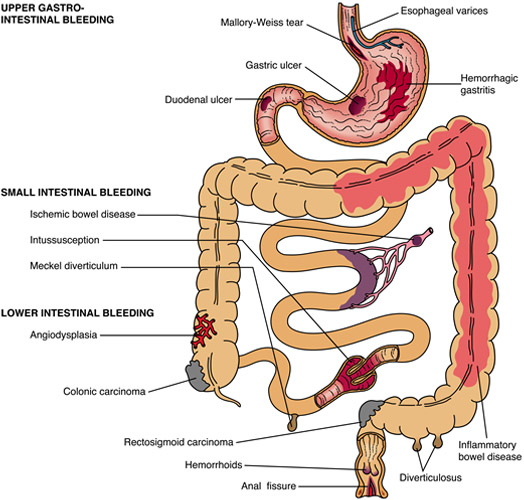
Your digestive or gastrointestinal (GI) tract includes the esophagus, stomach, small intestine, large intestine or colon, rectum, and anus. Bleeding can come from any of these areas. The amount of bleeding can be so small that only a lab test can find it.
Signs of bleeding in the digestive tract depend where it is and how much bleeding there is. GI bleeding is a symptom of a disease or condition, rather than a disease or condition itself.
Acute GI bleeding is sudden and can sometimes be severe. Chronic GI bleeding is slight bleeding that can last a long time or may come and go.
Symptoms of gastrointestinal (GI) bleeding may include
- Black or tarry stool
- Bright red blood in vomit
- Cramps in the abdomen
- Dark or bright red blood mixed with stool
- Dizziness or faintness
- Feeling tired
- Paleness
- Shortness of breath
- Vomit that looks like coffee grounds
- Weakness
- Acute bleeding symptoms: You may go into shock if you have acute bleeding. Acute bleeding is an emergency condition. Symptoms of shock include: a drop in blood pressure, little or no urination, a rapid pulse, unconsciousness. If you have any symptoms of shock, you or someone should call Doctor.
To diagnose gastrointestinal (GI) bleeding, a doctor will first find the site of the bleeding based on your medical history—including what medicines you are taking—and family history, a physical exam, and diagnostic tests.
Diagnostic tests:
Depending on your symptoms, your doctor will order one or more diagnostic tests to confirm whether you have GI bleeding and, if so, to help find the source of the bleeding.
Lab tests:
Lab tests to help diagnose the cause of your GI bleeding include Stool tests to detect occult bleeding and blood tests to detect whether you have anemia.
Endoscopy:
Endoscopy procedures involve a doctor examining a hollow passage in your body using a special instrument. An endoscopy procedure may help your doctor see if and where you have GI bleeding and the bleeding’s cause. Doctors most often use upper GI endoscopy and colonoscopy to test for acute GI bleeding in the upper and lower GI tracts.
Imaging tests:
Abdominal CT scan. An abdominal computerized tomography (CT) scan uses a combination of x-rays and computer technology to create images of your GI tract. An x-ray technician performs the procedure in an outpatient center or a hospital. A radiologist reads and reports on the images.
Angiogram. An angiogram is a special kind of x-ray in which a radiologist threads a catheter through your large arteries. The radiologist performs the procedure and interprets the images in a hospital or an outpatient center. You may receive a light sedative to help you stay relaxed and comfortable during the procedue.
Treatment of gastrointestinal (GI) bleeding depends on the cause and location of your bleeding.
Surgery:
During an upper GI endoscopy, a lower GI endoscopy, a colonoscopy, a flexible sigmoidoscopy, or a laparotomy, a doctor can stop the bleeding in your GI tract. He or she can stop the bleeding by inserting tools through an endoscope, colonoscope, or sigmoidoscope to inject medicines into the bleeding site, treat the bleeding site and surrounding tissue with a heat probe, an electric current, or a laser, close affected blood vessels with a band or clip. When a person has severe acute bleeding or bleeding that does not stop, a surgeon may need to perform a laparoscopy or a laparotomy to stop the bleeding
Endovascular Treatment:
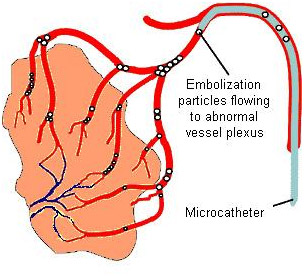
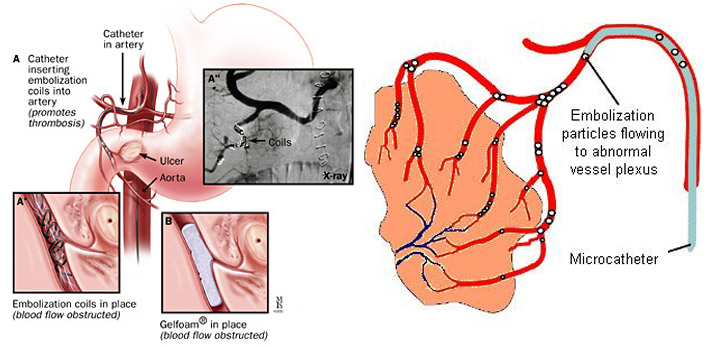
During an angiogram, a radiologist can inject medicines or other materials into blood vessels to stop some types of bleeding called embolisation.Nonvaricealupper gastrointestinal bleeding and arterial lower gastrointestinal bleeding remains an often serious clinical challenge. Catheter guided Embolisation by interventional radiologists is important in treatment. With improvements in catheter-based therapy and endovascular device development, angiography and embolization procedures is considered the gold standard for acute Nonvaricealupper gastrointestinal bleeding and arterial lower gastrointestinal bleeding refractory to endoscopy. It is a safe and effective alternative to surgery.
Medicines:
When infections or ulcers cause bleeding in your GI tract, health care professionals prescribe medicines to treat the problem.
The treatment of choice for massive Nonvaricealupper and lower gastrointestinal arterial bleedingrefractory to endoscopyis selective embolisation of affected arteries, a minimally invasive technique performed by an interventional radiologist. The interventional radiologist inserts a catheter into the patient’s femoral vein (in the upper thigh) using fluoroscopy for guidance. The interventional radiologist then directs the catheter to the affected arteriessupplying gastrointestinal tract and inserts embolisation materials into the distal braches of arteries responsible for the bleeding to block the area, stopping the bleeding. The patient will have an angiography after the embolisation procedure to confirm if the procedure has been successful.
The treatment has high rates of immediate clinical success. If the bleeding recurs, the embolisation procedure can be repeated.
You will already have undergone some tests including a computed tomography (CT) scan to identify the area of bleeding. You may also have had a endoscopy. You will be an inpatient for the procedure. You may be asked not to eat for four hours before the procedure. If you have any allergies or have previously had a reaction to the dye (contrast agent), you must tell the radiology staff before you have the test.
A specially trained team led by an interventional radiologist within the radiology department. Interventional radiologists have special expertise in reading the images and using imaging to guide catheters and wires to aid diagnosis and treatment.
In the angiography suite or theatre; this is usually located within the radiology department. This is similar to an operating theatre into which specialised X-ray equipment has been installed.
You will be asked to get undressed and put on a hospital gown. A small cannula (thin tube) will be placed into a vein in your arm. The procedure will take place in the X-ray department and you will be asked to lie flat on your back. You may have monitoring devices attached to your chest and finger and may be given oxygen. Your groin area will be swabbed with antiseptic and you will be covered with sterile drapes. Local anaesthetic will be injected into the skin in your groin and a needle will be inserted into the artery. A fine plastic tube called a catheter will be placed into the artery. The radiologist uses X-ray equipment to guide the catheter towards the arteries that are bleeding in your gut. A special X-ray dye (contrast agent) is injected into the catheter to ensure a safe position for embolisation. The interventional radiologist can then block the abnormal arteries by carefully injecting tiny particles through the catheter guided by images on a screen. Small amounts of contrast are injected down the catheter to check that the abnormal arteries are blocked satisfactorily. Once the interventional radiologist is satisfied with the images, the catheter will be removed. Firm pressure will be applied to the skin entry point, for about ten minutes, to prevent any bleeding. Sometimes a special device may be used to close the hole in the artery.
Every patient is different, and it is not always easy to predict; however, expect to be in the radiology department for about two hours.
You will be taken back to your ward. Nursing staff will carry out routine observations including pulse and blood pressure and will also check the treatment site. You will stay in bed for at least six hours. You will be kept in hospital overnight and may be discharged the next day.
