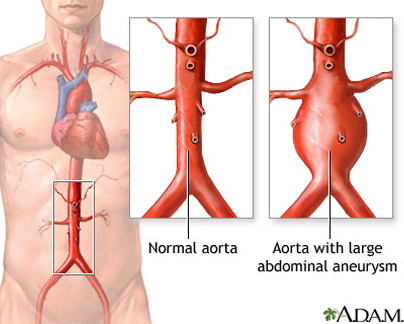
Aortic aneurysms (AA) are caused by progressive weakening of the aortic wall creating a “ballooning” of the vessel. The aneurysm will grow larger and eventually rupture if it is not diagnosed and treated. Aneurysms occur most often in the aorta, the main artery of the chest and abdomen. The aorta carries blood flow from the heart to all parts of the body including the vital organs and the legs and feet.
Proteins in the wall of the aorta, called elastin and collagen provide strength and flexibility to this large artery. This is similar to muscles and tendons providing strength to the arms and legs. Aneurysms are caused by a progressive breakdown of these proteins that lead to a weakness of the wall of the aorta that can steadily expand like a balloon. These proteins, collagen and elastin, may gradually deteriorate with age. Inflammation that is associated with atherosclerosis (hardening of the arteries) helps to accelerate this degenerative process even in younger people. Some of the body’s naturally occurring enzymes may also cause the breakdown of collagen and elastin in the wall of the aorta. An excess of these enzymes or conditions that activate the enzymes may cause the formation of an aneurysm, or lead to its sudden growth. In rare cases an aneurysm may be caused by infection. There is still much to be learned about the cause of aneurysms and their growth.
- Age over 60 years
- Family history of AA
- Tobacco use
- History of heart disease or peripheral artery disease
- High blood pressure (hypertension)
Abdominal Aortic Aneurysms
Most abdominal aortic aneurysms (AAAs) develop slowly over years. They often don’t cause signs or symptoms unless they rupture. If you have an AAA, your doctor may feel a throbbing mass while checking your abdomen.
When symptoms are present, they can include:
- A throbbing feeling in the abdomen
- Deep pain in your back or the side of your abdomen
- Steady, gnawing pain in your abdomen that lasts for hours or days
If an AAA ruptures, symptoms may include sudden, severe pain in your lower abdomen and back; nausea (feeling sick to your stomach) and vomiting; constipation and problems with urination; clammy, sweaty skin; light-headedness; and a rapid heart rate when standing up.Internal bleeding from a ruptured AAA can send you into shock. Shock is a life-threatening condition in which blood pressure drops so low that the brain, kidneys, and other vital organs can’t get enough blood to work well. Shock can be fatal if it’s not treated right away.
Thoracic Aortic Aneurysms
A thoracic aortic aneurysm (TAA) may not cause symptoms until it dissects or grows large.
If you have symptoms, they may include:
- Pain in your jaw, neck, back, or chest
- Coughing and/or hoarseness
- Shortness of breath and/or trouble breathing or swallowing
A dissection is a split in one or more layers of the artery wall. The split causes bleeding into and along the layers of the artery wall.If a TAA ruptures or dissects, you may feel sudden, severe, sharp or stabbing pain starting in your upper back and moving down into your abdomen. You may have pain in your chest and arms, and you can quickly go into shock.
A ruptured aneurysm is an emergency and procedures must take place immediately to save one’s life and avoid serious complications.
Although abdominal aortic aneurysm can be detected by physical examination, most are aneurysmsdiagnosed today using an ultrasound scan or CAT scan. These are simple, non-invasive exams conducted on an outpatient basis. These exams also measure the size ofAA, a key element in determining the best treatment. When aneurysms are diagnosed early, treatment is safe and effective and the aneurysm is curable. Aneurysms are often detected while performing tests for entirely different reasons. Most patients have no symptoms, so if you are at risk, it is important to discuss aortic aneurysm with your doctor.
If the aortic aneurysm is larger than 5 centimeters in diameter (about the size of a lemon), it will require treatment. Your interventional radiologist’s decision to treat will be based on the risk of the aneurysm rupturing, along with procedure risks, and risks associated with other pre-existing conditions. Smaller aneurysms that cause back, chest pain or abdominal pain may also need treatment, especially for those that are enlarging rapidly.
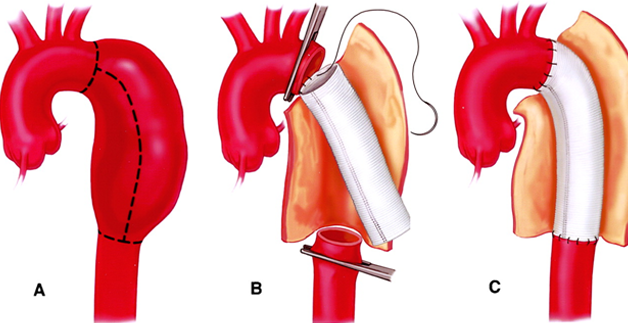
Surgical treatment
During the surgery, the surgeon makes an abdominal or chest incision, then replaces the diseased part of the aorta with a Dacron or Teflon graft that is carefully matched to the normal aorta. This graft is sewn in place by the surgeon. Most patients stay in the hospital for five to ten days if no complications occur. Complete recovery from the operation may take one to two months before returning to a full and normal life. It is a very durable procedure but operative risk is very high.
Less Invasive Treatments of aortic aneurysms,
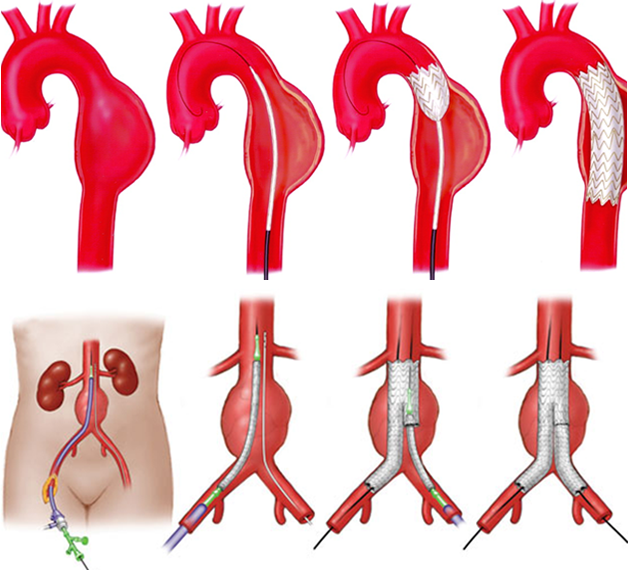
Endovascular aortic repair (EVAR)
Recent advances in catheter-based technologies have led to exciting new treatments for aortic aneurysms. Now, endovascular grafting technology allows the repair of the aortic aneurysms by inserting a graft through a small incision in the groin. The endovascular method allows the graft to be delivered through a catheter or tube inserted in a groin artery. X-ray guidance is then used to accurately position the graft in the aortic aneurysm. The graft is then expanded inside the aorta and held in place with metallic hooks rather than sutures. The hospital stay is usually only one or two days, and most patients can return to work or normal daily activities in about a week. Patients with other medical problems or those that could not withstand major surgery can be considered for repair by an endovascular graft. Endovascular grafting may not be possible in every case. Endovascular grafts are specially manufactured and don’t “fit” everyone’s anatomical situation. Speak with our expert interventional radiologist about the best option for you. The combination of early diagnosis with safer, simpler, and ever more successful treatments can prevent deaths due to ruptured abdominal aortic aneurysms.
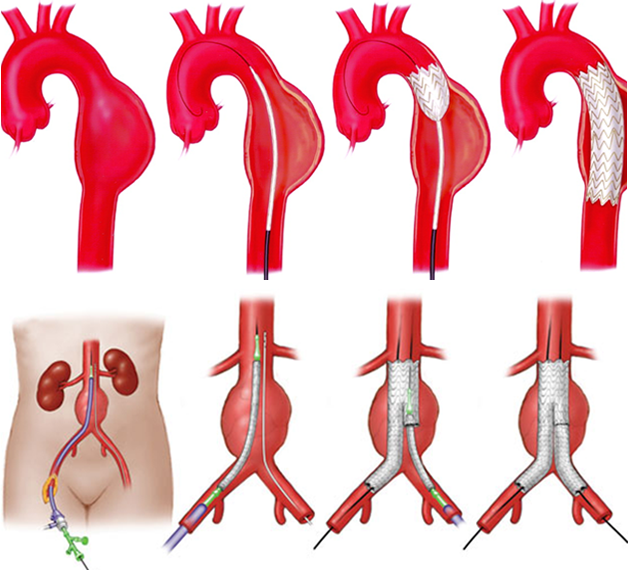
Endovascular aortic repair (EVAR) is a way of repairing an abnormality in the main blood vessel leaving your heart (aorta) by inserting covered metal mesh tubes (stent grafts). Stent grafts are typically inserted in a minimally invasive manner via the arteries in you groin using X-ray guidance to position them accurately. It is an alternative procedure to the conventional open surgical repair of the aorta.
You will have already had imaging, either a computed tomography (CT) or a magnetic resonance imaging (MRI) scan, to look at the aorta in your abdomen. The tests have shown that the aorta in your abdomen is enlarged and has developed an aneurysm. The size of the aneurysm is such that there is a risk of it bursting (rupture). This is a very serious problem and most people will not survive a rupture. Repairing the aorta before it ruptures usually has good results. Repair can either be done with a major surgical operation to replace the abdominal aorta with a ‘plastic tube’ or the aorta can be ‘relined’ from the inside with a stent graft.Both procedures work well, with EVAR being a less significant procedure. Not all patients with an aneurysm are suitable for EVAR, but imaging has shown that yours is.
EVAR is a major but normally safe procedure. There are a number of risks and complications that can arise. They are relatively rare; some are less than a major surgery, others are about the same. There can be damage to the blood vessels through which the tubes are placed or damage to the aneurysm causing a leak. This may require other radiological procedures or conversion to a major surgical repair. Occasionally, because of the size of your blood vessels, it may not possible to insert the stent graft satisfactory and surgical conversion may also be required. These complications are uncommon. The stent graft may not completely seal the aneurysm, allowing it to continue to fill. Small leaks are quite common and usually require no additional treatment. Some larger leaks may require a further procedure to seal them. There are small risks related to the anaesthetic which will be explained to you by your anaesthetist.
You need to be an inpatient for the procedure. You may be asked not to eat for four hours before the procedure, although you may still drink clear fluids such as water. If you have any allergies or have previously had a reaction to the dye (contrast agent), you must tell the radiology staff before you have the test. The procedure can be carried out with a variety of anaesthetic techniques ranging from a full general anaesthetic to a needle in your back to numb your lower body (spinal). The anaesthetist will explain the various options and risks.
A team of doctors, including a vascular surgeon and a specially trained doctor, called an interventional radiologist, performs the procedure. Interventional radiologists have special expertise in reading the images and using imaging to guide catheters and wires to aid diagnosis and treatment.
In the angiography suite or theatre; this is usually located within the radiology department. This is similar to an operating theatre into which specialised X-ray equipment has been installed. Some centres perform the procedure within a surgical theatre with a mobile X-ray machine.
You will have whatever anaesthetic is best for you. Before the EVAR, the vascular surgeon and interventional radiologist will explain the procedure and ask you to sign a consent form. Please feel free to ask any questions that you may have. You will be asked to get undressed and put on a hospital gown. A small cannula (thin tube) will be placed into a vein in your arm. The procedure is performed under sterile conditions and the interventional radiologist and a vascular surgeon will wear sterile gowns and gloves. Small incisions are made in your groin to expose the artery. Once the artery is exposed within the groin, a special guide wire and catheter (fine plastic tube) will be inserted into the artery and guided to the correct position to obtain the images required. The stent graft is introduced from the groin and positioned using the X-ray equipment; dye (contrast agent) is injected into the blood vessels to check the position. Once the aneurysm is satisfactorily excluded, the tubes and wires are removed and the arteries in the groin closed with stitches.
Every patient is different, and it is not always easy to predict; however, on average the anaesthetic and procedure will take two or three hours.
You will be returned to a special unit to recover from the anaesthetic. You will then normally go to a dependency unit for close observation for approximately 24 hours. You should be fit for discharge after 3–5 days.
There is a small chance that your aneurysm will continue to fill after a stent graft is inserted or the graft may move. It is, therefore, important that this is checked regularly with CT or MRI imaging. The first scan will be soon after the insertion with increasing intervals thereafter.
