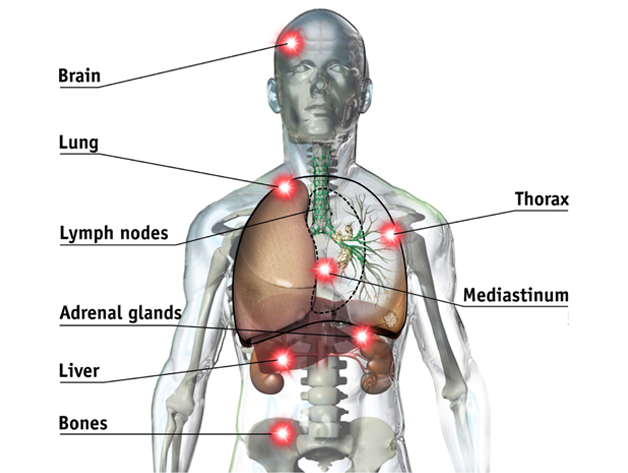
Normally, cells grow and divide to form new cells as the body needs them. Old cells eventually die and new cells take their place. Sometimes, this orderly process goes wrong: new cells form when the body does not need them and old cells do not die when they should. These extra cells can form a mass of tissue, known as a tumor. Cancerous tumors are abnormal and divide without control or order. Metastases occur when a single tumour cell or clump of cells spread into the bloodstream or lymphatic system, travel to a new organ, multiply and then regrow their vascular structure to obtain a supply of blood for delivery of nutrients.
Interventional oncology (abbreviated IO) is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. It is a rapidly evolving field where innovative techniques for diagnosing and treating cancer result in prolonged quality survival for patients with cancer.
While the surgical excision of tumors is generally accepted to offer the best long-term solution, it is often not possible due to the size, number or location of the tumor. Interventional oncology therapies may be applied to shrink the tumor, making a surgical or interventional treatment possible. Some patient groups may also be too weak to undergo open surgery. Interventional oncology treatments can be applied in these complex cases to provide effective and milder forms of treatment. Interventional oncological techniques can also be used in combination with other treatments to help increase their efficacy. For example, Interventional oncology techniques can be used to shrink large tumors making them easier to excise. Chemotherapeutic drugs can also be administered intra-arterially, increasing their potency and removing the harsh effects of system-wide delivery.
Patients can greatly benefit from Interventional oncology treatments. The minimally invasive nature of the treatments means they cause less pain, fewer side effects and shorter recovery times.
Many Interventional oncology procedures can be performed on an outpatient basis, freeing up hospital beds and reducing costs.
Therapeutic Procedures
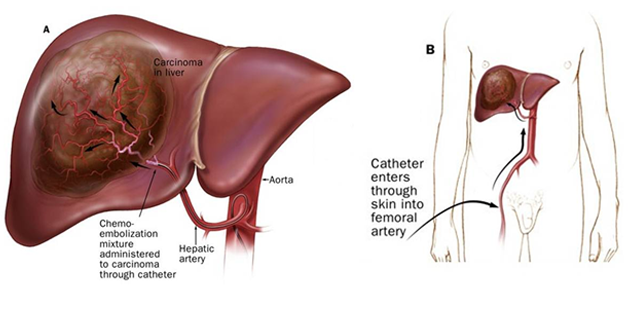
- Intraarterial ProceduresChemoembolization (TACE) and (DEB):
Chemoembolization is a method used to deliver chemotherapy medication directly to liver tumors — either primary tumors that originated in the liver, or metastases that migrated to the liver from cancers at other sites. Even in cases where chemoembolization is not curative, this approach may relieve a patient’s symptoms and extend survival.Doctors begin the procedure by inserting a catheter into a blood vessel in the patient’s groin and advancing it into the specific artery supplying the liver. The doctor then injects a dye and visualizes the tumor and blood vessels on an x-ray to determine the condition of the portal vein (a major blood vessel in the liver) and assess blood supply to the tumor.The physician then injects an emulsion of anticancer drugs and radiopaque oil through a catheter selectively placed into the artery feeding the tumor. This mixture keeps a high concentration of medication in contact with the tumor for a period of time longer than that associated with traditional systemic chemotherapy. After the treatment is administered, the catheter is withdrawn, and the patient can usually return home after an overnight stay in the hospital.Chemoembolization offers several advantages over traditional systemic chemotherapy: Prolonging the time the medication stays in contact with the tumor — up to as much as a month — increases the treatment’s effectiveness. Moreover, because the medication is delivered only to the tumor — rather than administered throughout the patient’s bloodstream — healthy tissues are spared from side effects, allowing doctors to administer dosages that are up to 200 times greater than those used in conventional chemotherapy. The substances that are part of the injected mixture not only hold the medication in place, but also block the blood supply to the tumor — depriving it of oxygen and nutrients and thereby halting its growth.RadioembolizationRadioembolization, is a technique, similar to chemoembolization, which allows delivery of localized treatment to primary or metastatic liver tumors. Whereas chemotherapy medication is the treatment delivered into the arteries supplying the tumors during chemoembolization, during Radioembolization the medication injected into these arteries consists of tiny beads coated with a radioactive material, Yttrium-90. These beads become lodged in the tumors. The radiation from these beads gradually decreases over the next 2 week, all while continuously destroying the cancerous cells. The tumor killing radiation from these beads travels only 1/16” through tissue so it does not travel outside of the patient’s body. This targeted approach to radiation delivery, allows much higher treatment radiation doses to be directly and safely delivered to the tumor than conventional radiation. This enables pin point delivery of radiation protecting the surrounding normal tissues.
- Tumor ablation
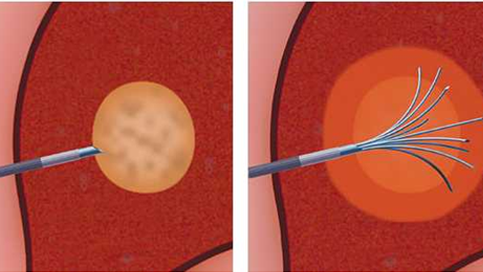
Tumor AblationDoctors are also using interventional radiology techniques to apply heating, freezing, or substances such as acetic acid or ethanol directly into tumors as a means of killing cancer cells. This type of treatment, called tumor ablation, is a relatively new technique that is showing promising results for treating cancer.
Cryoablation
Radiofrequency ablation (RFA)
Microwave ablation
Supportive Procedures
Relief of Obstructions
Some cancers can grow to the point where they obstruct the normal flow of urine or bile, causing these fluids to build up in the body. Without treatment, such obstructions can cause not only pain, but possibly infection or even liver or kidney failure. Doctors can insert an x-ray-guided catheter into the obstructed area to drain excess fluids. They may also choose to insert a stent — a tiny wire mesh tube — into the organ to bypass the obstruction and permit fluids to drain normally.
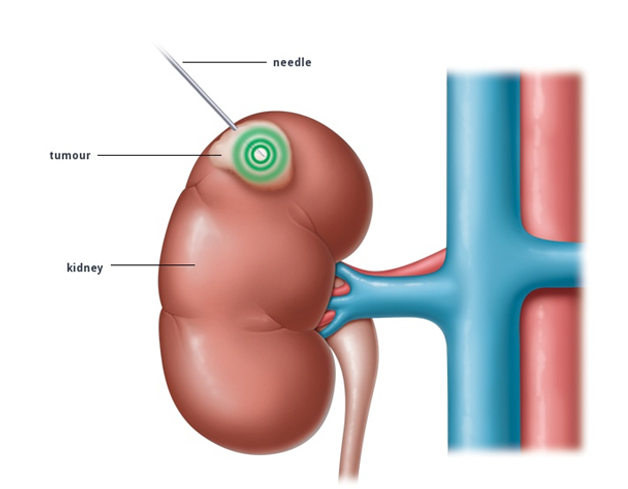
Tumor Biopsy
Many cancers are now diagnosed by needle biopsy. During this procedure, a doctor uses imaging techniques (such as CT, x-ray, ultrasound, or MRI) to guide the insertion of a fine needle into a patient’s tumor. A small amount of tissue is removed and then examined by a pathologist to determine if cancer cells are present. Needle biopsies are less painful, less disfiguring, and result in a shorter recovery time than conventional surgical biopsy procedures.
Others:
- Paracentesis or Thoracentesis
- PICC line placement
- Tunneled catheter placement
- Port catheter placement
- Percutaneous biliary drainage
- Percutaneous nephrostomy
- Pleurx catheter placement
- Stenting of malignant strictures: bile duct, esophageal, tracheobronchial and intestinal
- Portal vein embolization
Generally, interventional oncology is meant for patients who have not responded to chemotherapy or radiation, cannot receive more radiation, are unable to undergo surgery and/or need relief from their cancer pain. It is also used as a “bridge” for certain cancer patients who are waiting for an organ transplant.
Interventional radiologists treat the following cancers with these interventional procedures:
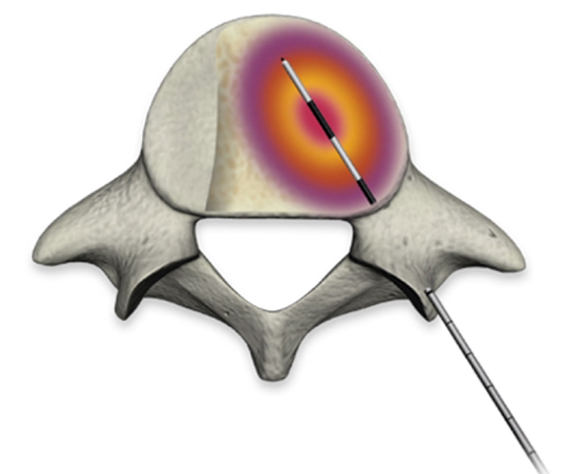
Bone cancer
- Radiofrequency ablation (RFA)
- Cryoablation (CA)
- Vertebral augmentation (cementoplasty)
Kidney cancer
- Cryoablation (CA)
Liver cancer
- Chemoembolization
- Cryoablation (CA)
- Radioembolization
- Radiofrequency ablation (RFA)
- Microwave ablation
- Irreversible Electroporation (IRE)
Lung
- Radiofrequency ablation (RFA)
- Microwave ablation
- Irreversible Electroporation (IRE)
It has a number of benefits for patients
- Rapid relief from symptoms.
- The imaging techniques allow accurate diagnosis and treatment using cutting-edge equipment. Diagnosis is reconfirmed during procedure.
- Minimally invasive procedures are performed through a small hole in the skin, minimising the patient’s discomfort and recovery time. There won’t be any scar.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay. As interventional procedures tend to require only local anaesthesia, hospital stays are very short, with patients frequently going home the day the procedure is performed.
- Patients who undergo IR procedures experience less pain during and after the procedure than patients undergoing surgical procedures. Post-procedural care is provided, along with follow-up imaging to confirm if the treatment has been successful.
- Minimal damage to surrounding vital anatomical structures with no significant structural weakness.
- No or negligible blood loss. No requirement of blood transfusion.
- Return to work and other normal activities usually within the first few days after the procedure.
- Low risk compared to surgery. The techniques can be used in very sick patients who are unfit for surgery.
- Overall procedure is less expensive than surgery or other alternatives.
