Acute limb ischemia (ALI) occurs when there is a sudden lack of blood flow to a limb. Acute limb ischemia is caused by embolism or thrombosis. Thrombosis is usually caused by peripheral vascular disease (atherosclerotic disease that leads to blood vessel blockage), while an embolism is usually of cardiac origin. With proper intervention, acute limb ischaemia is a highly treatable condition; however, delayed treatment (beyond 6 to 12 hours) can result in permanent disability, amputation, and/or death. Therefore, timely and correctly treatment of this disease is important.

Acute limb ischaemia can occur in patients through all age groups. Patients that smoke and have diabetes mellitus are at a higher risk of developing acute limb ischemia. Most cases involve people with atherosclerosis problems.
Symptoms of acute limb ischaemia include:
- Pain
- Pallor
- Paresthesias
- Perishingly cold
- Pulselessness
- Paralysis
These symptoms are called the six P’s. They are commonly mis-attributed to compartment syndrome. One more symptom would be the development of gangrene. Immediate medical attention should be sought with any of the symptoms. In late stages, paresthesia is replaced by anesthesia due to death of nerve cells. In some cases, gangrene can occur within six hours of ischemia. If patient is fully anesthetic and paralyzed, it is often too late to save the limb.
Absolute contraindications
CVA/TIA in last 2 months
Active bleeding
Recent GI bleeding-last 10 days
Neurosurgery in last 3 months
Intracranial trauma in last 3 months
Relative contraindications
CPR in last 10 days
Major non vascular surgery or trauma in last 10 days
Uncontrolled HTN >180/110
Puncture of non compressible vesse
Intracranial tumor
Recent eye surgery
 Percutaneous catheter-directed thrombolytic therapy is defined as the process of percutaneous thrombus lysis with the use of special designed interventional equipment and can be achieved currently by simple pharmacological or combined pharmacomechanical thrombolysis. Pharmacological thrombolysis is herein defined as the process of thrombus dissolution through the selective catheter-directed infusion of thrombolytic agents. Mechanical thrombolysis (thrombectomy) is herein defined as mechanical disruption of the thrombus. Pharmacomechanical thrombolysis is herein defined as the mechanical disruption of the thrombus combined with pharmacological thrombolysis.
Percutaneous catheter-directed thrombolytic therapy is defined as the process of percutaneous thrombus lysis with the use of special designed interventional equipment and can be achieved currently by simple pharmacological or combined pharmacomechanical thrombolysis. Pharmacological thrombolysis is herein defined as the process of thrombus dissolution through the selective catheter-directed infusion of thrombolytic agents. Mechanical thrombolysis (thrombectomy) is herein defined as mechanical disruption of the thrombus. Pharmacomechanical thrombolysis is herein defined as the mechanical disruption of the thrombus combined with pharmacological thrombolysis.
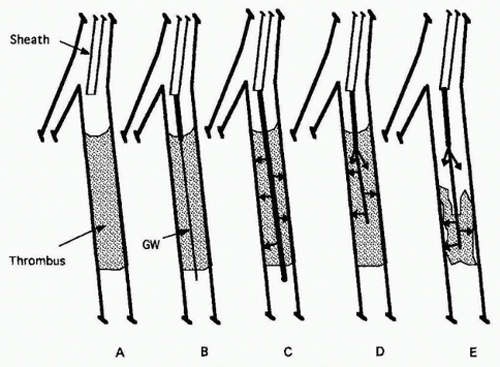
Stages of IA thrombolysis.
A: An occluded segment of vessel is demonstrated arteriographically.
B: A coaxial catheter is introduced through the IA sheath and advanced into the proximal thrombus, and a guidewire is then advanced to the distal end of the thrombus.
C: A tip-occluded multiside-orifice catheter is advanced into the entire thrombus, which is saturated with a lacing dose of lytic agent deposited by rapid pulse-spray infusion. (Alternatively, an end-hole catheter or a catheter with fewer distal side-holes is advanced distally and then retracted proximally while depositing small doses of lytic agent at each site.)
D: Continuous infusion is administered with an end-hole catheter with its tip in the proximal thrombus and a smaller side-hole catheter that is advanced much farther into the clot. (A distal untreated segment of thrombus is shown here, but a side-hole catheter, with its tip occluded, may be advanced so as to bathe the thrombus with lytic agent throughout its length.)
E: As thrombolysis progresses, both catheters may be advanced, but with this configuration, the inner catheter alone may be advanced into the receding thrombus front. The process continued until the entire thrombus is dissolved and an underlying obstructing lesion is uncovered for treatment by angioplasty or surgery.
