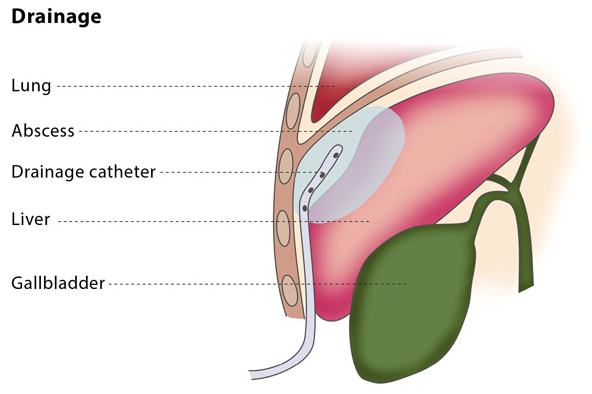
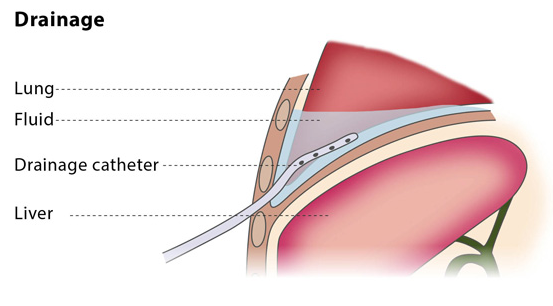
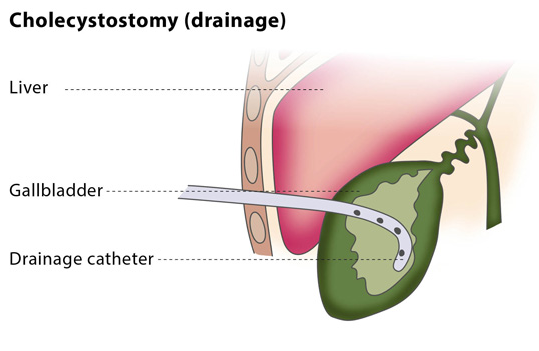
Image-guided percutaneous drainage involves using a catheter (a thin tube) to drain an abscess or a collection of fluid or air under image guidance. The interventional radiologist will insert a flexible catheter through a small cut in your skin and will guide the catheter to the collection of fluid or air. The fluid or air will then be collected in a drainage bag.
Drainage catheters are available in a variety of sizes, shapes and types. The interventional radiologist will choose the catheter according to the type of fluid, along with other factors.
If you are on any medication that prevents blood clotting, you will stop taking it before the procedure, if possible.
You should not eat anything for at least four hours before the procedure starts. You may be asked to fast for longer, depending on the puncture and difficulty of your particular case. Before the procedure, the interventional radiologist will usually place a needle in your vein to make access easier during the procedure.
Most drainage procedures are performed under local anaesthesia or conscious sedation, so you will be awake but feel no pain. You may be asked to take antibiotics beforehand to reduce the risk of infection, but this is uncommon. You will lie down for the procedure – the exact position you will be asked to lie in depends on the access route that the interventional radiologist will use to safely approach the lesion.
According to the location of the fluid/air collection or abscess, the interventional radiologist will choose an imaging technique, such as ultrasonography, CT, magnetic resonance or fluoroscopy.
The procedure will be carried out in a sterile and safe environment. The interventional radiologist will use a direct puncture to place a hollow needle called a trocar.
Percutaneous drainage can be performed as an in-patient or out-patient procedure. The puncture site and your vital signs will be monitored for 4-6 hours. You will experience some mild discomfort around the puncture site in the first few hours after the procedure.
The interventional radiologist will periodically follow up using imaging to confirm that the abscess or fluid collection has gone.
Percutaneous drainage is recommended to treat fluid or air collections which produce symptoms (such as pneumothorax, which is the collection of air or gas in the gap between the chest wall and the lungs). It can also treat recurrent fluid collections by using medication and is a minimally invasive method of draining abscesses.
This procedure may not be suitable for you if you suffer from a blood clotting disorder or if the interventional radiologist cannot find a safe access route for the catheter.
The percutaneous drainage procedure cures infected fluid/air collections in over 80% of patients, though failure occurs in 5-10% of patients.
Because of the wide range of types of uninfected collections, the success rate of drainage for uninfected collections is highly variable.
There are some risks associated with the procedure. Major complications include bacteraemia (the presence of bacteria in the blood, which occurs in 2-5% of cases) and septic shock (caused by severe infection and sepsis, which occurs in 1-2% of cases). Other complications include the risk of haemorrhage and superinfection (infection of a sterile collection of fluid, following a previous infection).
