Your arteries deliver oxygen -rich blood from your heart to other parts of your body. Your peripheral arteries carry blood away from the heart to your arms and legs. The peripheral arteries in your legs are extensions of the largest artery in your body, the aorta. The aorta travels down through your abdominal region and branches off into the iliac arteries of each leg.
The iliac arteries further divide into smaller arteries and deliver blood down your legs to your toes. Healthy peripheral arteries are smooth and unobstructed, allowing blood to flow freely to the legs and provide oxygen, glucose, and other nutrients that your legs need.Typically with age, the peripheral arteries build up plaque, a sticky substance made up mostly of fat and cholesterol. Plaque narrows the passageway within the arteries and causes them to become stiff.
Peripheral arterial disease results when the peripheral arteries become too narrow or obstructed and limit the blood flow to the legs. If left untreated, peripheral arterial disease can cause pain or aching in the legs, difficulty with walking, resting pain in the foot at night in bed, non -healing sores or infections in the toes or feet, and can lead to limb loss in its most severe form. In addition, it can be associated with other serious arterial conditions leading to heart attacks and stroke.
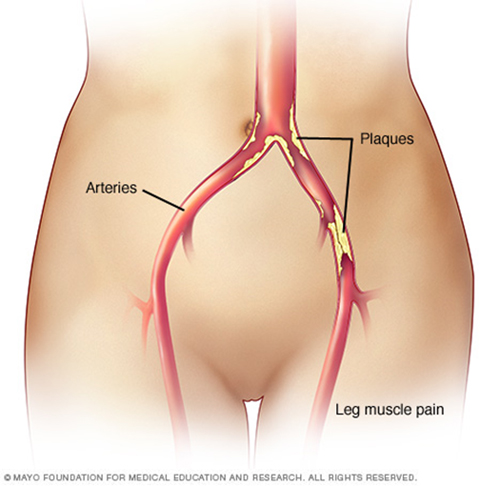
 PVD mainly affects blood circulation to the legs and feet. Many people with PVD do not have any symptoms (asymptomatic PVD). For people who have PVD with symptoms, the most common is pain in the legs, particularly the calves, when walking. The pain usually goes away within several minutes after stopping exercise.
PVD mainly affects blood circulation to the legs and feet. Many people with PVD do not have any symptoms (asymptomatic PVD). For people who have PVD with symptoms, the most common is pain in the legs, particularly the calves, when walking. The pain usually goes away within several minutes after stopping exercise.
Other symptoms may include:
- Numbness, weakness or a feeling of heaviness in the legs with no pain
- Hair loss on your feet and legs
- Poor nail growth (brittle toenails)
- Cool or shiny skin on your legs, or cold or numb toes
- A change in the colour of your legs
- A weak pulse in your legs or feet.
- Sores or ulcers on your toes and feet that do not heal properly
- Pain in the legs while resting
- Pain in the feet or toes while resting, especially when lying flat.
- Old Age
- Hypertension (high blood pressure)
- Diabetes
- Smoking
- High cholesterol
- Obesity
- Lack of exercise
- Family history of vascular problems
After that, other tests may be done. They include:
- Colour Doppler
- CT angiogram (CTA)
- Magnetic resonance angiogram (MRA)
- Catheter angiogram (DSA)
Most people with PAD can be treated with lifestyle changes, medicines, endovascular treatment or rarely bypass surgery.
Lifestyle changes to lower your risk include:
- Stopping smoking (smokers are 4 times more likely to get PAD and have symptoms of PAD than nonsmokers.)
- Controlling diabetes
- Controlling blood pressure
- Being physically active (including a supervised exercise program)
- Eating a diet low in fat.
Drug treatment includes:
- Antiplatelet agents to prevent blood clots
- Cholesterol-lowering medicine (statins)
- High blood pressure medicine
Endovascular treatment includes:
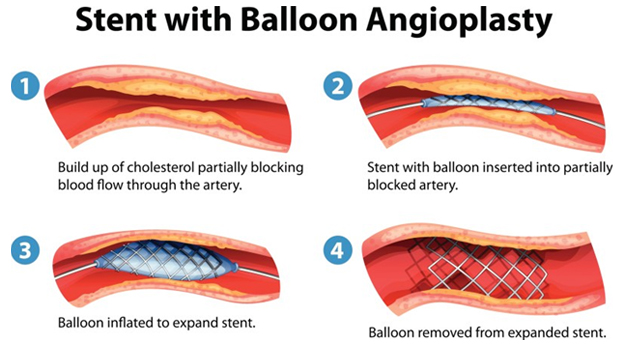
Angioplasty and Stenting: Angioplasty is a non-surgical procedure that widens narrowed or blocked arteries. A thin tube (catheter) with a deflated balloon on its tip is passed into the narrowed artery segment. Then the balloon is inflated. This pushes open the narrowed segment. Then the balloon is deflated and the catheter is withdrawn. Often a stent (a wire mesh tube) is placed in the narrowed artery with a catheter. There the stent expands and locks open. It stays in that spot, keeping the diseased artery open.
The Endovascular treatment generally takes few hours in a DSA suit with no scarring. Patients can usually resume normal activities next day with minimal or no pain. The success rate of the Endovascular treatment is high and measurably better than the bypass or vascular surgery.
It has a number of benefits for patients
- Rapid relief from symptoms.
- The imaging techniques allow accurate diagnosis and treatment using cutting-edge equipment. Diagnosis is reconfirmed during procedure.
- Minimally invasive procedures are performed through a small hole in the skin, minimising the patient’s discomfort and recovery time. There won’t be any scar.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay. As interventional procedures tend to require only local anaesthesia, hospital stays are very short, with patients frequently going home the day the procedure is performed.
- Patients who undergo IR procedures experience less pain during and after the procedure than patients undergoing surgical procedures. Post-procedural care is provided, along with follow-up imaging to confirm if the treatment has been successful.
- Minimal damage to surrounding vital anatomical structures with no significant structural weakness.
- No or negligible blood loss. No requirement of blood transfusion.
- Return to work and other normal activities usually within the first few days after the procedure.
- Low risk compared to surgery. The techniques can be used in very sick patients who are unfit for surgery.
- Overall procedure is less expensive than surgery or other alternatives.
