An angiogram is a special X-ray examination designed to show the arteries in your body relevant to your problems. A dye (contrast agent), which usually contains iodine, is injected directly into the artery through a fine tube (catheter). The dye fills the arteries and makes them more visible on an X-ray screen.
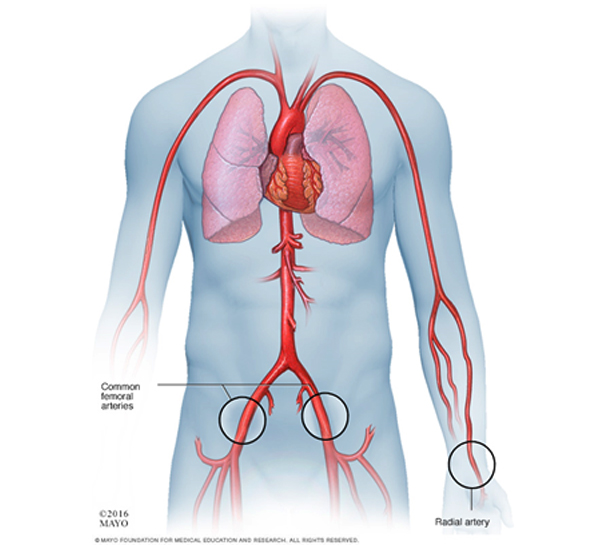
Your doctor needs detailed images of the arteries to determine the most appropriate treatment for you. Angiograms are most commonly performed to investigate blockages, areas of bleeding and to depict the blood supply to abnormal areas. Other tests such as a Doppler ultrasound scan, a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan may have been performed but your doctors have decided that more detailed information about your arteries is required.
Angiography is a very safe procedure, but as with any medical procedure there are some risks and complications that can arise. A small bruise (haematoma) around the site of the needle can occur, but this is quite normal. The bruise might be sore for a few days but will disappear in a few weeks. Rarely a large bruise may develop and require a small operation to drain it. Occasionally, a tender pulsating swelling called a false aneurysm may develop over a few days due to ongoing leakage from the arterial puncture site. This can usually be treated by an injection of a blood-clotting agent under ultrasound guidance. Very rarely, some damage can be caused to the artery by the catheter or by displacement of the material causing a blockage in other arteries (an embolus). This may require a small operation or another procedure.
The dye (contrast agent) used during the procedure is very safe, but occasionally can cause damage to the kidneys. This occurs mainly in patients whose kidney function is abnormal already and this will be identified on the blood tests that are performed before the procedure. Allergic reactions to the dye are also possible, but are very rarely serious.
An angiogram is usually carried out as a day case procedure under local anaesthetic. You may be asked not to eat for four hours before the procedure, although you may still drink clear fluids such as water. Before coming into hospital, you will have been asked about certain risk factors for vascular disease unless you have to come into hospital as an emergency. These factors include checking your blood pressure; your kidney function and making sure you are not on treatment for diabetes or blood clots. If you are taking warfarin, this may be stopped before the procedure and you may require admission to hospital to give you an alternative.
If you are diabetic, your doctors will advise you about any changes needed to your normal medication. If you have any allergies or have previously had a reaction to the dye (contrast agent), you must tell the radiology staff before you have the test.
A specially trained team led by an interventional radiologist within the radiology department. Interventional radiologists have special expertise in reading the images and using imaging to guide catheters and wires to aid diagnosis and treatment.
In the angiography suite or theatre; this is usually located within the radiology department. This is similar to an operating theatre into which specialised X-ray equipment has been installed.
Before the angiogram, the interventional radiologist will explain the procedure and ask you to sign a consent form. Please feel free to ask any questions that you may have and, remember that even at this stage, you can decide against going ahead with the procedure if you so wish. You will be asked to get undressed and put on a hospital gown. A small cannula (thin tube) may be placed into a vein in your arm. Occasionally, you may require a fluid drip to help your kidney function before the angiogram. You will be asked to lie on the X-ray table, generally flat on your back. The X-ray machine will be positioned above you.
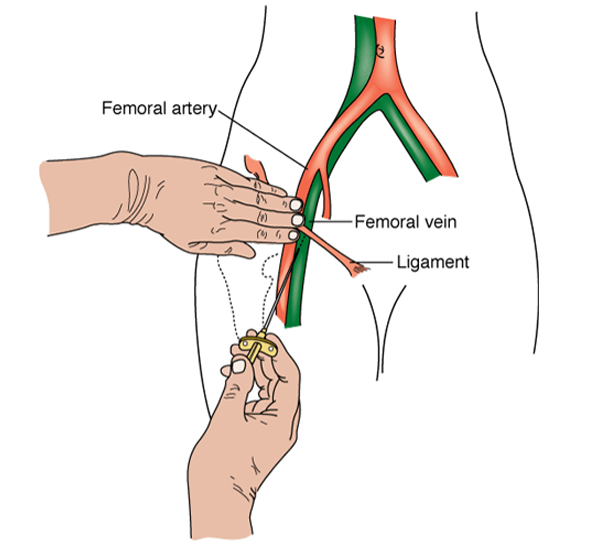
You may have monitoring devices attached to your chest and finger and may be given oxygen. An angiogram is performed under sterile conditions and the interventional radiologist and radiology nurse will wear sterile gowns and gloves to carry out the procedure. Your skin near the point of insertion, usually the groin area, will be swabbed with antiseptic and you will be covered with sterile drapes. The skin and deeper tissues over the artery will be numbed with local anaesthetic. A needle followed by a wire and catheter (fine plastic tube) will be inserted into the artery and guided to the correct position to obtain the images required.
This involves injecting small quantities of the dye (contrast agent) into the blood vessels. Once the interventional radiologist is satisfied with the images, the catheter will be removed. Firm pressure will be applied to the skin entry point, for about ten minutes, to prevent any bleeding. Sometimes a special device may be used to close the hole in the artery.
It may sting a little when the local anaesthetic is injected. You may feel a warm sensation for a few seconds when the dye is injected and feel like you are passing urine.
Every patient is different, and it is not always easy to predict; however, expect to be in the radiology department for about an hour.
You will be taken back to your ward. Nursing staff will carry out routine observations including pulse and blood pressure and will also check the treatment site. You will generally stay in bed for a few hours, until you have recovered and are ready to go home. Finally Some of your questions should have been answered by this leaflet, but remember that this is only a starting point for discussion about your treatment with the doctors looking after you. Make sure you are satisfied that you have received enough information about the procedure.

