Venous malformations are abnormally developed blood vessels with varying degrees of communication with normal veins. They are sometimes described abnormal ‘vascular lakes’ containing very slow moving blood. Supporting these vascular lakes is a solid component known as matrix. The ratio of spaces and matrix within a vascular malformation varies considerably from patient to patient. It can differ to some extent within different malformations within the same person. They are classified as low flow lesions meaning that they contain venous blood, which is very slow moving. Occasionally the blood moves so slowly that the blood can clot within the malformation. This usually leads to swelling and pain within the malformation.
They can occur anywhere in the body and are present at birth, although they may not become apparent until later in life. Other situations when they may become apparent are following episodes of local trauma, at puberty or pregnancy due to hormonal changes occurring at these times. Depending on their location venous malformations may cause pain, swelling, restriction of movement or cosmetic issues. Occasionally venous malformations can bleed especially if they are in a very superficial position. Treatment may be indicated because of the appearance or for associated functional problems.
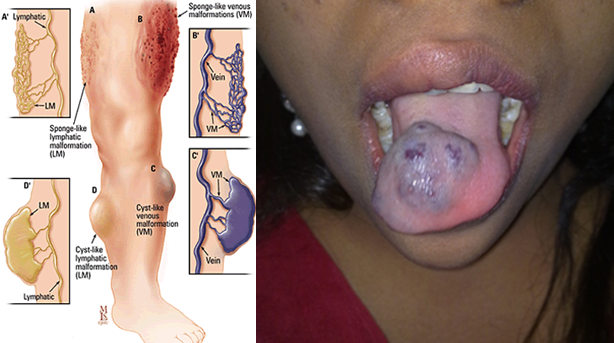

VMs have a wide range of appearances on imaging with ultrasound, Magnetic resonance or venography. They can range in the amount of matrix present, size of the vascular spaces and communication between spaces as well as the drainage network into the main venous system. There is no universally accepted classification system for low flow venous malformations
Typically the main symptoms encountered include pain and swelling. The swelling is typically dependent; by lowering the area affected to below the heart allows the lesion to swell. A significant number of venous malformations involve the skin giving a bluish discolouration. The bluish discolouration and swelling can lead to cosmetic issues depending on the site of the lesion. Intermittently the venous malformation can become painful, swollen and hard. This is mainly due to episodes of thrombosis (blood clot) within the lesion itself. These blood clots typically do not move to the lungs in the majority of circumstances.
At present there is nothing that can be done to prevent the development of a venous malformation but there are several forms of treatment available. These types of lesions usually occur spontaneously and are not inherited and cannot be passed on to children. There are several syndromes that can have a familial tendency but these are extremely rare.
Your doctor will have a suspicion or a good indication that you have a venous malformation on the basis of the history you provide and on physical examination or in some circumstance your family history. Your doctor will refer you to a specialist.
The diagnosis is typically clinical and imaging the lesion is key to understand the size and nature of the lesion. Imaging can also help decide when and how to treat these lesions. Ideally VMs should be managed by a ‘multi-disciplinary’ team of doctors, nurses and specialists with a specific interest and experience in diagnosing and treating this condition. The most useful imaging for low flow VMs is ultrasound and MRI, however occasionally a CT has been performed. The appearance of venous malformations are usually typical on MRI, however occasionally can look different and a biopsy may be required to confirm the diagnosis and exclude other more sinister causes that may present similarly to venous malformations.
Ultrasound: Is a very useful imaging test that can be performed in clinic to assess the VM, especially its morphology of spaces to matrix. It is very helpful in assessing suitability for treatment.
CT Scan: This is not routinely performed but can demonstrate the presence of multiple calcified foci consistent with phleboliths commonly seen in low flow VMs.
MRI scan: This is the most useful imaging for low flow VMs. They are often known as “iceberg lesions” in that what you see is only the tip. MRI is able to demonstrate the total extent of the underlying malformation.
Treatment options are divided up in to conservative management, percutaneous injections or surgery or a combination of these. If there are no symptoms then there is no indication or need for treatment.
Initially it important to determine the exact symptoms and to what degree this is distressing the patient and how much of an impact this is having on their life. The majority of venous malformations do not need treatment, but this can be reviewed at any time, especially if symptoms worsen or change. Venous malformations are not malignant and do not have malignant potential.
Conservative management includes pain relief with anti-inflammatory tablets, compression dressings if the lesion is in a limb and alteration of lifestyle accordingly. This approach is usually advised if symptoms are well tolerated.
Treatment depends on the number of vascular spaces within the lesion and the amount of more solid tissue. Lesions with a more spacious component (ie: more venous lakes) are more suitable for injection therapy or ‘sclerotherapy’ than those that are predominantly solid in nature. Depending on the site, size amongst other factors certain lesions are suitable for surgical removal.
Treatment options will be discussed in the multidisciplinary clinic with the patients’ opinion taken into account.
Sclerotherapy is a type of treatment that involves the injection of a special chemical into the venous malformation to ultimately shrink it and relieve the symptoms it is causing. Various substances can be used but most commonly the chemical used is Sodium Tetradecylsulphate (Fibrovein). When injected into a lesion it causes an inflammatory reaction which leads to localised blood clots and the formation of a scar in place of the venous malformation. This corresponds to shrinkage of the malformation. This is carried out under ultrasound and x-ray control as the doctor needs to be sure that the correct part of the malformation is accessed with the needle and needs to assess the degree of communication with adjacent communicating veins.
Often a ‘course’ of multiple injections are required to adequately treat a venous malformation and it can be some time before the patient notices a significant difference. Not all venous malformations are successfully treated in this way but in the vast majority of cases significant results are achieved. Sclerotherapy is not a ‘cure’ for these malformations but is aimed at symptom control and reduction in size. Sclerotherapy may not treat skin discolouration associated with some malformations. It is typically carried out as a day case procedure in hospital.

Immediately after the injection considerable swelling can occur along with pain. This usually settles within days – weeks of the injection. Pain is usually adequately treated with oral pain killers. It is when this swelling settles that there is a noticeable reduction in the size and / or symptoms of the malformation.
There is a small risk of infection and bleeding but as sclerotherapy is carried out via a needle puncture and not an incision this is unusual.
There is a small chance that the skin over the malformation will breakdown and lead to a blister or even a small ulcer, but this will improve in time and possibly leave a scar. This is more common in superficial malformations that involve the skin or occupy a large area directly under the skin (subcutaneous). Surgical revision of sclerotherapy induced scars is an option should this be required.
If a malformation is near a nerve or group of nerves the swelling induced by sclerotherapy can sometime compress the nerve and stun it. This can lead to loss of sensation in the area or even local muscle weakness; this can for example occur in facial lesions but is uncommon. This condition is termed ‘neuropraxia’ and if it occurs at all is often temporary and is rarely permanent.
General anaesthetic is often required for sclerotherapy and this carries a small risk.
These are the general risks and the multidisciplinary team will discuss more specific risks to an individual according to the size, site and type of malformation.
