Lung cancer refers to the uncontrolled cell growth in lung tissue. The leading risk factor for lung cancer is exposure to tobacco smoke, with smoking accounting for 80-90% of lung cancer cases. Other causes of lung cancer include genetic factors, asbestos exposure and air pollution.
Primary lung cancer, which starts in the lung, usually originates from cells that help protect or enclose organs. The lungs are the most common site for primary cancer worldwide. Metastatic lung disease, on the other hand, is when cancerous cells spread to the lung from other parts of the body, and is also common.
Lung cancer has a variety of symptoms, including persistent coughing, wheezing and shortness of breath, as well as coughing up blood, especially in smokers. You may also notice weight loss, fever, fatigue and deformities in the fingers and fingernails, which are referred to as clubbing.
Compression and invasion of structures near the tumour can also cause other symptoms, including chest pain, hoarseness, and swelling of the face and neck if there is a blockage preventing blood flowing back to the heart (resulting in a condition called superior vena cava obstruction).
There are a number of tests which can be used to diagnose lung cancer. The first step often involves the doctor taking a chest X-ray, and an imaging technique called CT may be used to provide more details about the type, location and extent of the disease.
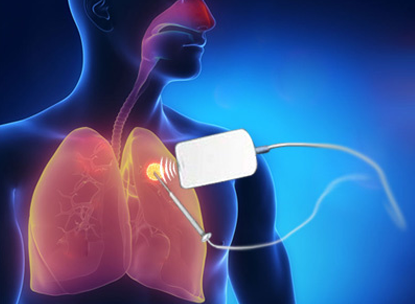
In most cases, a specialist will also have to perform a biopsy to obtain and examine a tumour sample. This is usually done by way of a bronchoscopy, where the specialist inserts a narrow tube (scope) through your mouth or nose and windpipe, into your lungs, and then takes small tissue samples using a tiny device. It can also be done with an image-guided needle biopsy, where the specialist uses CT for guidance while moving a needle to the area from which a sample is taken.
If the cancer is in the very top of a lung and the specialist suspects that it has invaded the network of nerves in your neck and chest (called the brachial plexus) or your vascular system, you may undergo an imaging procedure called MRI.
A further way of detecting some types of cancerous cells is an imaging technique called positron emission tomography (PET), which involves injecting a small amount of a tracer that travels through your blood, collects in organs and tissues, and allows the specialist to see certain areas of concern more clearly.
The treatment options available to the patient depend on the specific characteristics of the cancer, including its cell type, location, whether or not it has metastasised and how well the patient’s heart and respiratory system are working.
Surgery is considered the main curative treatment. If surgery is not an option for a patient, and the disease is limited to the lung, an interventional technique called image-guided ablation can play a major role. This procedure involves an interventional radiologist using image guidance to insert a needle into the tumour. The tumour is destroyed by delivering radiofrequency energy (radiofrequency ablation), microwave heat (microwave ablation) or a gas that freezes the tissue (cryoablation).
Patients who suffer from small cell lung carcinoma or incurable cancer can improve the quality and length of their lives by undergoing chemotherapy and radiotherapy (in which high-energy X-rays are aimed at the site of the cancer).
- Rapid relief from symptoms.
- The imaging techniques allow accurate diagnosis and treatment using cutting-edge equipment. Diagnosis is reconfirmed during procedure.
- Minimally invasive procedures are performed through a small hole in the skin, minimising the patient’s discomfort and recovery time. There won’t be any scar.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay.As interventional procedures tend to require only local anaesthesia, hospital stays are very short, with patients frequently going home the day the procedure is performed.
- Patients who undergo IR procedures experience less pain during and after the procedure than patients undergoing surgical procedures. Post-procedural care is provided, along with follow-up imaging to confirm if the treatment has been successful.
- Minimal damage to surrounding vital anatomical structures with no significant structural weakness.
- No or negligible blood loss. No requirement of blood transfusion.
- Return to work and other normal activities usually within the first few days after the procedure.
- Low risk compared to surgery. The techniques can be used in very sick patients who are unfit for surgery.
- Overall procedure is less expensive than surgery or other alternatives.
