Renal artery stenosis is a narrowing of arteries that carry blood to one or both of the kidneys. Most often seen in older people with atherosclerosis (hardening of the arteries), renal artery stenosis can worsen over time and often leads to hypertension (high blood pressure) and kidney damage. The body senses less blood reaching the kidneys and misinterprets that as the body having low blood pressure. This signals the release of hormones from the kidney that lead to an increase in blood pressure. Over time, renal artery stenosis can lead to kidney failure.
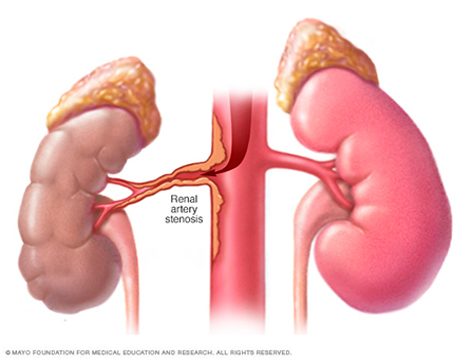
Renal artery stenosis can lead to several different clinical syndromes ranging from difficult to control hypertension to recurrent pulmonary edema (shortness of breath due to the lungs filling with fluid) to ischemic nephropathy (kidney dysfunction due to compromised arterial blood flow) and frank renal failure. Renal artery stenosis is most often due to severe atherosclerotic plaque build-up in the renal arteries (typically in those over age 50) but may be due to fibromuscular dysplasia (FMD) seen more frequently in women under the age 50.
The prevalence of renal artery stenosis is increased in diabetics with high blood pressure and in those with known coronary and peripheral arterial disease.
Secondary hypertension, which has an identifiable cause, is usually suspected in children, adolescents and young adults when there is an abrupt onset of high blood pressure. It also frequently occurs in patients, whose high blood pressure is poorly controlled despite usual therapy, including medications. In these cases, renal artery stenosis can be detected by physical examination or special tests:
- A physician’s examination of the upper abdomen with a stethoscope may detect the abnormal sounds of turbulent blood flow through narrowed renal arteries.
- An Abdominal Ultrasound examination can detect abnormal blood flow to and within the kidneys.
- Magnetic Resonance Imaging (MRI) can display narrowed regions in the renal arteries.
- X-Ray Arteriography involves injection of a dye into the arterial system. It shows the location and extent of narrowing, which is necessary to determine whether the stenosis is severe enough to warrant treatment.
- Surgery: Surgical removal or by-pass of the narrowing in the renal artery. Surgery is rarely done due to significant periprocedure risk.
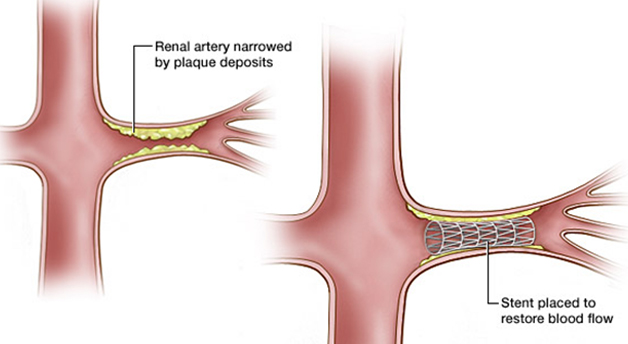
- Renal artery angioplasty and stenting: Catheter-based endovascular treatment options include balloon angioplasty alone (usually reserved for cases of fibromuscular dysplasia) and more commonly angioplasty with stenting both with the goal of improving blood flow to the affected kidney which may ultimately aid in long-term blood pressure control and improving kidney function.
A renal artery is the main blood vessel to the kidney. A renal artery angioplasty and stent is done to treat a narrowed renal artery also called renal artery stenosis. Using X-rays as a guide, a small plastic tube is put into the narrowed artery. A special balloon on the tube is blown up to open the narrowed part of the artery. An expandable tube called a stent is then put in to keep the artery open.
You will be asked to lie flat on your back on the X-ray bed. Staff will clean the skin on your groin or arm and place sterile drapes over you. They will then inject a local anaesthetic, which may sting a little.
A special tube is put into the artery in the groin or arm and passed into the renal artery. The dye is injected through the tube. The tube is X-rayed to make sure it is in the right place. The tube is moved into the narrowed part of the artery and another tube is put in which has a tiny balloon on it. This will be inflated to widen the narrowed part of the artery.
A stent is then put in over the balloon. Once the stent is in the right place the balloon is inflated. The balloon tube is then taken out and the stent is left in the renal artery. The tiny hole in the artery in your groin or arm will be pressed by one of the staff for about 15 minutes to block it.
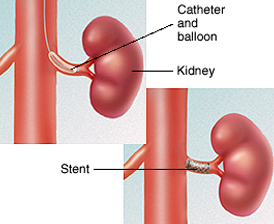
You will be taken back to your ward on a trolley and will usually need to stay in hospital overnight. The nurse will check your pulse and blood pressure a few times and check your groin or arm in case there is any bleeding.
You may be given aspirin or other blood thinning medication to stop clotting near the stent.
The wound on your groin or artery may be a little sore when you go home. You will be told how to look after this. Staff will need to take out the needle if it is still in your arm. Staff will give you any special instructions. The dye will pass out of your body in your urine. You will not notice it as it is colourless.Drink plenty of fluid to help get rid of the dye.
Angioplasty or stenting will improve the blood flow in your artery but it will not cure the underlying cause of the blockage – arteries may become narrow again (called restenosis), which is why it is important to follow the advice below.
Any patient with this arterial disease, no matter which arteries are affected, stands to benefit from eating a low fat diet, getting regular exercise, and controlling blood cholesterol.
Angioplasty improves artery blood flow for most people. But, results will depend on where your blockage was and how much blockage you may have in your other arteries. In many cases, you will be prescribed aspirin medication in an attempt to prevent the problem occurring again and to reduce the risk of other artery related diseases such as heart attack and stroke.
If you are a smoker, it is very important that you stop smoking. Smoking causes the arteries to become narrowed and can also cause the blood to clot more rapidly.
The risk of progression or recurrence of disease of the arteries and its complications can be reduced after angioplasty and/or stent insertion by simple lifestyle modifications including:
- Weight reduction and exercise
- Eating a healthy diet, which is low in saturated fats
- Elimination of smoking
- Controlling high blood pressure, Diabetes mellitus and high cholesterol. Medications to reduce blood cholesterol (“statins”) are usually recommended and started by either the GP or the hospital doctors
