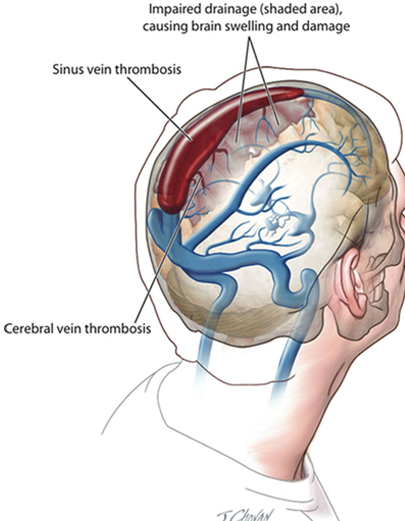
Blood drains from the brain into spaces called venous sinuses between the brain and skull. It then returns to the heart through veins.
In CVT, a blood clot forms in the venous sinuses. This blocks drainage of blood from the brain. As a result, blood cells may break and leak blood into the brain tissues, forming a hemorrhage that can be life- threatening.
CVT is rare, affecting approximately 2-4 in every million people each year. Many are younger people and most are female.
Cerebral venous sinus thrombosis is more common in particular situations. Most of these patients have at least one of these risk factors:
- Thrombophilia, a tendency to develop blood clots due to abnormalities in coagulation, e.g. factor V Leiden, deficiency of protein C, protein S or antithrombin, or related problems
- Nephrotic syndrome, a kidney problem causing protein loss in the urine
- Chronic inflammatory diseases, such as inflammatory bowel disease, lupus and Behçet’s disease
- Pregnancy and puerperium (the period after giving birth)
- Particular blood disorders, especially polycythemia vera and paroxysmal nocturnal hemoglobinuria
- Use of estrogen-containing forms of hormonal contraception
- Meningitis and infections of the ear, nose and throat area such as mastoiditis and sinusitis
- Direct injury to the venous sinuses
- Medical procedures in the head and neck area
- Sickle cell anemia
- Dehydration, primarily in infants and children
- Homocystinuria
Common symptoms are:
- Headache.
- Confusion, drowsiness, blacking-out.
- Stroke.
- Changes to feeling or moving your body.
- Seizures.
- Rarely some patients will have none of the usual symptoms.
- CVT patients are also at risk of deep vein thrombosis (DVT) and pulmonary embolism (PE).
- In DVT a blood clot forms in the leg. In PE this breaks away and travels into the lungs.
PE is a serious condition.
Possible symptomsdue to PE are:
- Chest pain
- Breathlessness
- Collapse
Doctors typically take a medical history and do a physical exam. Family and friends can describe the symptoms they saw, especially if the person who had the stroke is unconscious. The final diagnosis, however, is usually made based on how the blood is flowing in the brain. Imaging tests show areas of blood flow.
These tests may be used to diagnose venous sinus thrombosis:
- MRI scan
- CT scan
- Venography
- Angiography
- Ultrasound
- Blood tests
Treatment should begin immediately and must be done in a hospital. A treatment plan could include:
- Fluids
- Antibiotics, if an infection is present
- Antiseizure medicine to control seizures if they have occurred
- Monitoring and controlling the pressure inside the head
- Medicine called anticoagulants to stop the blood from clotting
- Surgery
- Continued monitoring of brain activity
- Measuring visual acuity and monitoring change
- Rehabilitation
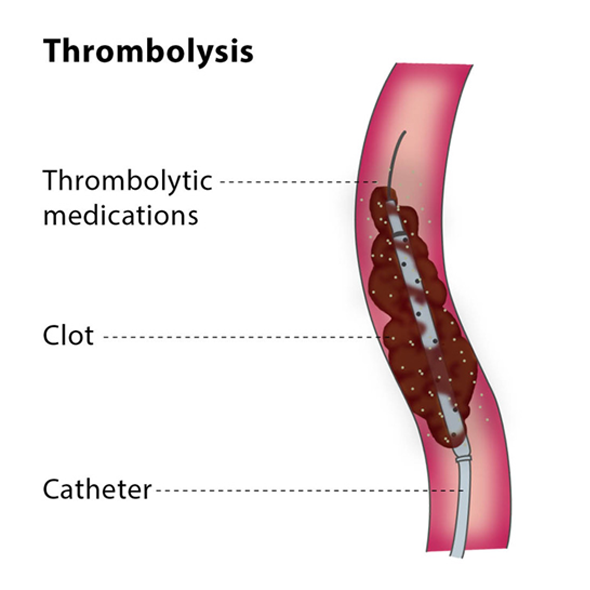
Despite intensive medical treatment and optimal anticoagulation, some patients develop progressive neurologic deterioration. In these patients probably there is a possible place for endovascular therapy.
Endovascular strategies involve super selective delivery of thrombolytic agents via several routes including transfemoral, transjugular, transcarotid, or directly through the venous sinus and mechanical thrombectomy. Higher recanalization rates have been reported with endovascular thrombolysis.
The present evidence suggests that endovascular therapy, both chemical thrombolysis and mechanical thrombectomy, may be a treatment option in patients who develop progressive deficit despite intensive medical treatment and optimal anticoagulation and have no intracerebral hemorrhage, elevated intracranial pressure or evidence of herniation.