Renal cell carcinoma is the most common type of kidney cancer. It occurs when cancerous cells grow in the tubules, which are small tubes in the kidney that filter and clean blood. Renal cell carcinoma is a collection of different types of tumors, each with their own identifying factors, rather than one single entity.
In general, tumors in the kidney are discovered either during routine screening or when patients experience symptoms due to the size or location of the renal cell carcinoma.
Common symptoms include blood in the urine, pain between the upper abdomen and back and anemia. Less commonly, patients experience weight loss, high blood pressure, or recurring fever.
A number of tests can help doctors diagnose renal cell cancer and assess the stage of the cancer. Imaging techniques include ultrasound, CT, MRI and PET.
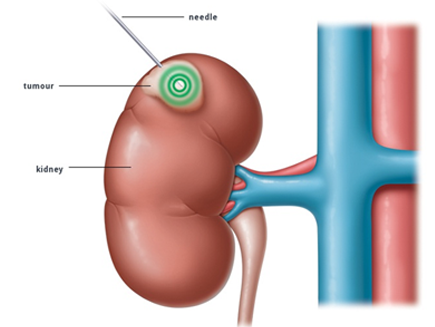
In most cases, a biopsy is necessary to determine the type of cancer and its aggressiveness. The tissue samples are commonly obtained by way of image-guided interventional techniques.
Surgery
There are a number of possible treatment options, including the surgical removal of all or part of the affected kidney. Traditionally, this involved removing the whole kidney, but removing part of the kidney has recently been shown to be effective in some patients.
Tumor Ablation
There are also interventional techniques which can be used to treat renal cell carcinoma, such as thermal ablation. In this procedure, an interventional radiologist uses image guidance to insert a needle directly into the tumour and then destroys cancerous cells by delivering radiofrequency energy, microwave heat, extremely cold gas or a high-voltage direct current.
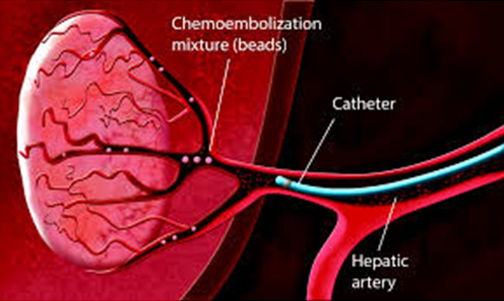
Chemoembolization
Some tumours are hypervascular, meaning that the amount of blood vessels in the tumour is higher than average. These tumours are especially hard to remove. For patients suffering from a hypervasculartumour, a procedure called transarterialchemoembolisation (TACE) may relieve pain and suffering. This procedure involves delivering a cancer-killing drug directly to a tumour whilst also depriving it of its blood supply, thus destroying the tumour.
It has a number of benefits for patients
- Rapid relief from symptoms.
- The imaging techniques allow accurate diagnosis and treatment using cutting-edge equipment. Diagnosis is reconfirmed during procedure.
- Minimally invasive procedures are performed through a small hole in the skin, minimising the patient’s discomfort and recovery time. There won’t be any scar.
- Most procedures can be performed on an outpatient basis or require only a short hospital stay. As interventional procedures tend to require only local anaesthesia, hospital stays are very short, with patients frequently going home the day the procedure is performed.
- Patients who undergo IR procedures experience less pain during and after the procedure than patients undergoing surgical procedures. Post-procedural care is provided, along with follow-up imaging to confirm if the treatment has been successful.
- Minimal damage to surrounding vital anatomical structures with no significant structural weakness.
- No or negligible blood loss. No requirement of blood transfusion.
- Return to work and other normal activities usually within the first few days after the procedure.
- Low risk compared to surgery. The techniques can be used in very sick patients who are unfit for surgery.
- Overall procedure is less expensive than surgery or other alternatives.
